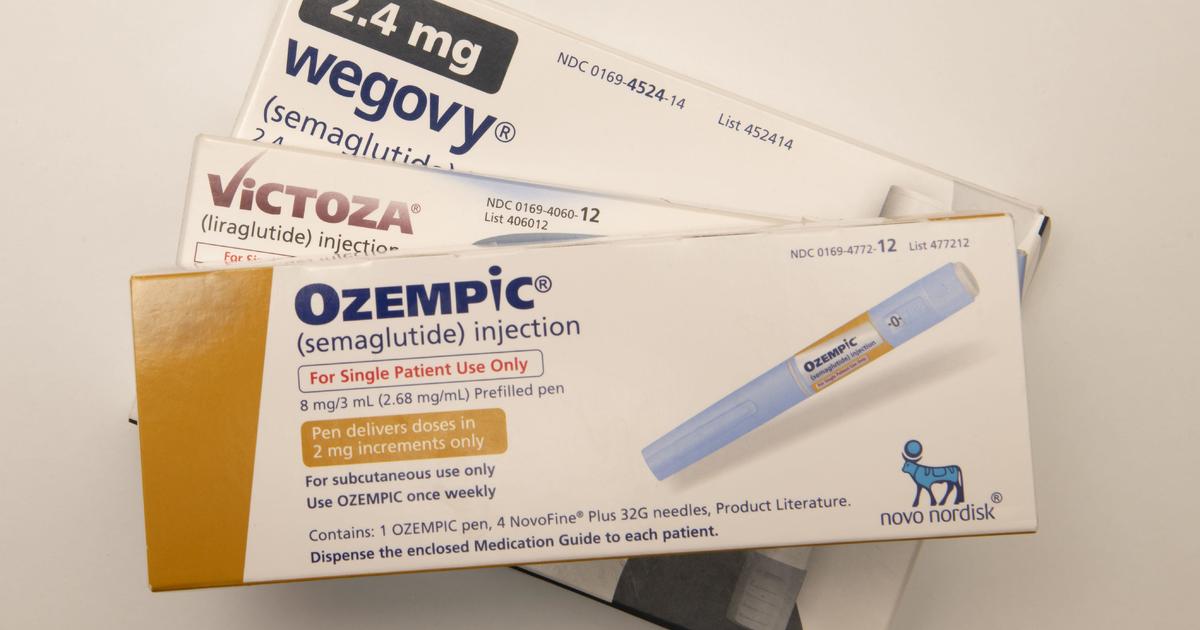
The Biden administration proposed a new rule that would make popular weight-loss drugs like Wegovy and Ozempic eligible for coverage by Medicare and Medicaid. This proposal, put forth by the U.S. Department of Health and Human Services, has the potential to benefit millions of Americans struggling with obesity. However, it also comes with a hefty price tag, estimated to cost taxpayers up to $35 billion over the next decade.
The introduction of this rule has sparked a debate between proponents of the weight-loss drugs and critics, such as Robert F. Kennedy Jr., who has been vocal about his opposition to these medications. As a nominee for a leadership position in the Department of Health and Human Services under the Trump administration, Kennedy may attempt to block the implementation of this rule.
Despite the potential cost, U.S. Health and Human Services Secretary Xavier Becerra believes that this proposal is a significant step forward for individuals battling obesity. He views it as a game-changer for those who would otherwise struggle to afford these medications. The White House has also expressed support for the proposal, stating that it would allow Americans and their doctors to make informed decisions about their health without financial barriers.
A bipartisan group of congressional members has advocated for the inclusion of weight-loss drugs in Medicare coverage, citing potential cost savings in treating chronic conditions related to obesity. By providing access to these drugs, the government could potentially alleviate the burden of treating obesity-related illnesses in the long run.
Under the proposed rule, Medicare and Medicaid coverage would be extended to individuals prescribed weight-loss drugs to address obesity. While most obese Medicare enrollees are already eligible for coverage due to other related conditions like diabetes or heart disease, the rule would expand coverage to around 7% of beneficiaries who were previously ineligible. However, individuals who are overweight but not obese would still need to have another qualifying condition, such as diabetes or heart disease, to be eligible for coverage.
The rule also affects state Medicaid programs, which would now be required to cover weight-loss drugs for obese residents. The Centers for Medicare and Medicaid Services estimate that 12% of adults covered by Medicaid would be newly eligible for coverage under this rule. Additionally, adolescents could also be covered, as the FDA has approved the use of Wegovy for individuals as young as 12 years old.
The market for anti-obesity drugs has seen significant growth in recent years, with the FDA approving a new class of weekly injectables like Wegovy and Zepbound to treat obesity. These medications work by mimicking hormones that regulate appetite, signaling fullness to the brain and gut when individuals consume food. Users of these drugs can experience weight loss ranging from 15% to 25% of their body weight.
However, the high cost of these drugs has been a point of contention. The proposal to include them in Medicare and Medicaid coverage raises questions about the financial impact on taxpayers and the healthcare system as a whole. Critics argue that the cost of covering these medications may outweigh the potential benefits, especially considering the long-term implications of widespread usage.
Overall, the proposed rule to include weight-loss drugs in Medicare and Medicaid coverage has the potential to significantly impact the lives of millions of Americans struggling with obesity. It represents a step towards addressing the healthcare needs of individuals battling weight-related conditions and could lead to improved health outcomes and cost savings in the long run. As the debate over the rule continues, it remains to be seen how it will ultimately shape the landscape of obesity treatment in the United States.